WHAT IS CERVICAL CANCER?
Cervical cancer is a malignant tumour that starts in the cells of the cervix. Malignant means that it can spread, or metastasize, to other parts of the body.
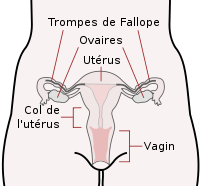
The cervix is part of a woman’s reproductive system. It is the narrow lower part of the uterus, or womb. It is the passageway that connects the uterus to the vagina.
Cells in the cervix sometimes change and no longer grow or behave normally. These changes may lead to non-cancerous, or benign, tumours such as polyps, cysts or fibroids.
Read more : http://www.cancer.ca/en/cancer-information....

WHAT IS ITS ORIGIN ?
The main cause of cervical cancer is a persistent infection with a virus that is sexually transmitted : the human papillomavirus or HPV (human papillomavirus). When this virus settles durably in the cervix, it can cause changes in the epithelium, it is called precancerous lesions. In rare cases, these lesions may progress to cancer. This evolution is slow since a cancer usually appears 10 to 15 years after the persistent infection by the virus.
-
SYMPTOMS
Cervical cancer may not cause any signs or symptoms in its early stages. Symptoms often appear once the tumour grows into surrounding tissues and organs. Other health conditions can cause the same symptoms as cervical cancer.
See your doctor if you have these symptoms:
- pale, watery, pink, brown or bloody discharge from the vagina between periods
- unusually long or heavy periods
- bleeding after sexual intercourse
- bleeding or bloody discharge from the vagina after menopause
- bleeding after a pelvic exam or vaginal douching
- pain during sexual intercourse
- increased amount of discharge from the vagina
- foul-smelling discharge from the vagina
Late symptoms develop as the cancer grows larger or spreads to other parts of the body, including other organs. Late symptoms of cervical cancer include:
- difficulty urinating
- loss of bladder control (called incontinence)
- blood in the urine (called hematuria)
- difficulty having a bowel movement
- blood in the stool
- constipation
- leaking of urine or feces from the vagina
- pain in the pelvic area or lower back that may go down one or both legs
- edema, or swelling, of the legs
- anemia (a reduction in the number of healthy red blood cells)
- weight loss
- shortness of breath
- bone pain
- fatigue (extreme tiredness or lack of energy)
- loss of appetite
Read more: http://www.cancer.ca/en/cancer-information/cancer-type/... -
DIAGNOSIS
Usually, diagnosing cervical cancer begins when a Pap test suggests a problem with the cervix. Your doctor will ask you about any symptoms you have and do a physical exam. Based on this information, your doctor will refer you to a specialist or order tests to check for cervical cancer or other health problems.
The process of diagnosis may seem long and frustrating. It’s normal to worry, but try to remember that other health conditions can cause similar symptoms as cervical cancer. It’s important for the healthcare team to rule out other reasons for a health problem before making a diagnosis of cervical cancer.
Read more: http://www.cancer.ca/en/cancer-information/cancer-type... -
TREATMENT
The choice of treatments is adapted to your situation, that is to say to the specific characteristics of the cancer of which you are affected. Several doctors of different specialties meet to discuss the best possible treatments in your situation (multidisciplinary consultation meeting). They are based on recommendations of good practice. They can also suggest you to participate in a clinical trial.
Treatment may include a combination of different treatments. When deciding which treatments to offer for cervical cancer, your healthcare team will consider:
- the stage
- your age
- your general health
- whether or not you want to become pregnant in the future
- your personal preferences
The treatment of cervical cancer depends on the extent of the disease, surgery, external radiotherapy, brachytherapy and chemotherapy, alone or in combination. Surgery is mainly used to treat tumors limited to the cervix, less than 4 centimeters. It most often involves removing the uterus, some of the surrounding tissues and organs, and the lymph nodes. Concomitant chemoradiotherapy combining external radiotherapy, brachytherapy and chemotherapy is the standard treatment for tumors larger than 4 centimeters and for tumors that have spread beyond the cervix into the pelvis. In the case of tumors that have reached distant organs (metastasis), the treatment is based on chemotherapy and / or radiotherapy (most often external). -
FOLLOW-UP
Follow-up after treatment is an important part of cancer care. Follow-up for cervical cancer is often shared among the cancer specialists (gynecologist, radiation oncologist, medical oncologist and surgical oncologist) and your family doctor. Your healthcare team will work with you to decide on follow-up care to meet your needs.
Don’t wait until your next scheduled appointment to report any new symptoms and symptoms that don’t go away. Tell your healthcare team if you have:
- pain in the pelvis, hips, back or legs
- bleeding or discharge from the vagina
- Changes in bowel habits or bladder function
- unexplained weight loss
- a cough that doesn’t go away
The chance of cervical cancer recurring is greatest within 2–3 years, so close follow-up is needed during this time. Smoking is a risk factor for cervical cancer, so women who have cervical cancer are strongly encouraged to stop smoking.
Read more: http://www.cancer.ca/en/cancer-information/cancer-type/cervical/treatment/follow-up/?region=on#ixzz5LC8pBAsr -
HPV VACCINES
These vaccines put on the market since 2006 are:
• Cervarix is on the market. It would only protect strains 16 and 18 responsible for 70% of cervical cancers. It is said bivalent. (GlaxoSmithKline).
• Gardasil is offered to girls from 9 to 26 years old. It is only effective as a preventative against HPV types 6, 11, 16, 18. It is therefore said quadrivalent. (Merck in the USA associated with Sanofi Pasteur in Europe).
In total, these 2 vaccines prevent only 75% maximum cervical cancer. The remaining 25%, more serious, are due to more rare strains. The duration of immunity conferred by vaccines is not known. The side effects of the vaccine in real life and long term are not known. They are still the subject of discussion among specialists.
The vaccines protect against 4 strains of papillomavirus, the 16 and 18, responsible for more than 7 out of 10 cervical cancers and the 6 and 11, responsible for genital warts. The overall goal is vaccination of 70-80% of 14-year-old girls before their first sexual intercourse to reduce the risk of cervical cancer by 70% and the condyloma acuminate by 90%.
The vaccine can be offered between the ages of 15 and 23, provided that young women have not had more than one sexual partner. Three injections are necessary. Both boosters must be done within 12 months of the first injection. They are usually recommended the second month and the sixth month. The vaccine does not provide protection against all carcinogenic HPVs, nor against existing infections.
The Pap smear remains unavoidable: The maintenance of screening for women aged 25 to 65 is essential in parallel with vaccination because the vaccine is not supposed to replace the smear. The HPV viral test makes it possible to detect the risk of cervical dysplasia or the presence of cancer in the event of permanent presence of the HPV virus. The risk seems to be eliminated for the next 5 or 10 years, if the test is negative. This test must be repeated every 3 years.